Temporomandibular Joint, TMJ
The person has two temporomandibular joints which work together as a pair, one in front of each ear. The joints connect the lower jaw bone (the mandible) to the temporal bones of the skull on each side of the head. The muscles controlling the joints are attached to the mandible and allow the jaw to move in three directions: up and down, side to side, and forward and back.
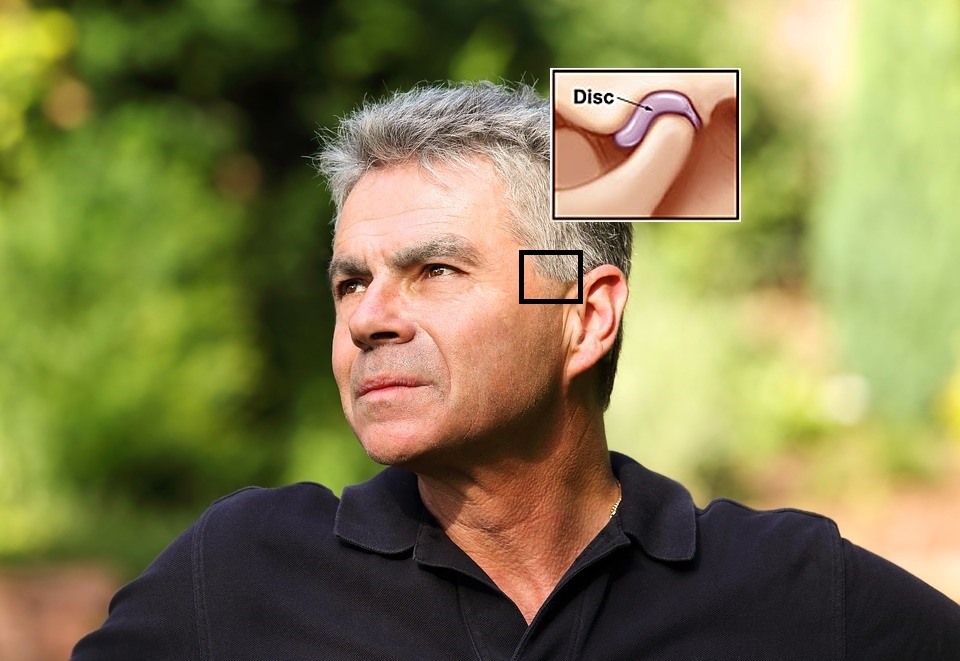
When you open your mouth, the rounded upper ends of the mandible on each side of the jaw (the condyles) glide along the joint socket at the base of the skull. They slide back to their original position when you close your mouth. To keep this motion working smoothly, a soft tissue disc lies between the condyle and the socket. The disc absorbs the shock to the joint from chewing and other movements.
The combination of synchronized as well as three-dimensional movements of the paired joints distinguishes them as the most complicated joints in the body.
Temporomandibular Joint Disorders, TMD
TMD often causes severe pain and discomfort in the jaw joint and surrounding tissues. It might affect one or both sides of your face and it can be temporary or last many years.
Temporomandibular Disorders (TMD) can affect a person’s ability to speak, chew, swallow, make facial expressions, and, in the most difficult cases, even breathe.
According to the world-wide statistics as well as practices, TMD is the most common among people between the ages of 20 and 40. TMD is diagnosed more often to women than men (from 6 to 9 times more often acc. to the different sources).
Causes that may affect TMD
In one cases one cause can be found as well as in other cases the full complex of causes that influence temporomandibular joint dysfunction or pathology. These are the cases when complex treatment decisions should be made. In some cases, no obvious cause can be found.
There can be stated multiple causes that may affect TMD:
- grinding or clenching yourteeth, which puts a lot of pressure on the joint;
- irregular or altered occlusion (it requires the individual estimation);
- movement of the soft cushion or disc between the ball and socket of the joint;
- infections;
- injuries to the jaw area;
- various forms of arthritis.
Symptoms of Temporomandibular Joint Dysfunction (TMD)
The symptoms, that are mentioned the most often by patients with TMD:
- pain in jaw sphere could vary acc. to the individual case – it could be intensive and barely perceptible as well as temporary or last for many years;
- limited movement or locking of the jaw
- painful clicking, popping or grating in the jaw joint when opening or closing the mouth
- ear pain, pressure, fullness, ringing in the ears (tinnitus), when otolaryngologists (the specialists of ear, nose and throat) cannot find any case for it;
- a bite that feels “off”
Occasional clicking or discomfort in the jaw joint is quite common and is not always a cause for concern. The problem often goes away on its own in several weeks to months. However, if the pain is severe and lasts more than a month, consult the maxillofacial surgeon.
Temporomandibular Joint (TMJ) Treatment
In order to evaluate the symptoms of possible TMJ dysfunction, the maxillofacial surgeon:
- makes sure your jaw works like it should and doesn’t lock when you open or close your mouth
- evaluates the movements of your jaw and the tension of the jaw muscles;
- listens for clicks, pops, or grating sounds and their frequency when the jaw is moves;
- evaluates occlusion.
The maxillofacial surgeon may take the further analyses such as detailed occlusion analyses, detailed analyses of TMJ movements, magnetic resonance imaging (MRI) or computer tomography (CT), additional consultations with other specialists. The treatment plan is discussed with the patient after the detailed analyse of the situation and, if it is necessary, the surgical treatment is applied.
The treatment plan and process depend on complains, subjective and objective causes that could influence TMJ disorders. There are no clear guidelines for the successful treatment of TMJ in the worldwide practise. This is why it is really important to use the practise of the best worldwide specialists of this sphere.
TMJ treatment could be divided into three directions:
- Conservative treatment;
- Conservative or surgical treatment (there are some cases when the patient has a possibility to choose the kind of treatment after the doctor’s explanation of few possibilities);
- Surgical treatment or surgical treatment after conservative treatment (in cases when the sufficient result is not reached with conservative treatment).
TMD cases are often very individual. The treatment plan is based on the existing problems and the expected result. The treatment possibilities and plan could be discussed just during the consultation with the maxillofacial surgeon.
Open Jaw Surgery may be done when:
- TMJ pain is very strong,
- limited movement, locking of the jaw or dislocation of the jaw is found,
- the problem cannot be solved with conservative or low invasion methods,
- other indications are found.
It is important to know that an open jaw surgery methods and incisions could vary and depends on the Maxillofacial Surgeon’s technique, theoretical and practical knowledge, the expected result and other criteria, that could be very individual.
To compare TMJ standard surgery methodology and a small access methodology the incision may vary even 3-4 times.
TMJ arthroscopy (TMJ Arthroscopic Surgery) –
is a surgical procedure that is performed on the TMJ or jaw joint that involves using a small, bendable tube with a camera on the end to see inside the jaw and make other procedures.
The arthroscopic surgery may be done for the purpose to:
- evaluate the real situation of TMJ (Temporomandibular Joint),
- remove scar tissue and thickened cartilage,
- influence the inflammatory zones,
- reposition the jaw disc,
- flush (lavage) the joint with special liquids,
- insert an anti-inflammatory medicine,
- reshape/change the surface of the jawbone,
- other procedures

